Constipation
WHAT IS CONSTIPATION?
Constipation is a condition where a person has trouble passing stool with ease.
SYMPTOMS OF CONSTIPATION
Very hard or dry lumpy stools that resemble sheep or rabbit droppings.
Straining, if you’re groaning, moaning, pushing, and straining to get anything to pass.
Infrequent bowel movements: The bowels open less than three times per week.
The feeling of incomplete evacuation, despite straining, with a feeling that there is poo left in there.
The sensation of obstruction or blockage, there feels like something is stopping the poo from moving through your bowel smoothly.
Spending too long in the toilet, taking more than a couple of minutes to pass a poo.
Pain in the rectum or anus.
Using fingers or toilet paper to remove stool or support the pelvic floor manually.
Abdominal pain or discomfort
Bloating or distension
Heartburn
Nausea
When constipated, stool may appear as small, hard pellets similar to sheep droppings.
WHAT IS A NORMAL POOp?
Characteristics of a healthy stool and bowel movements:
Shape & Consistency:
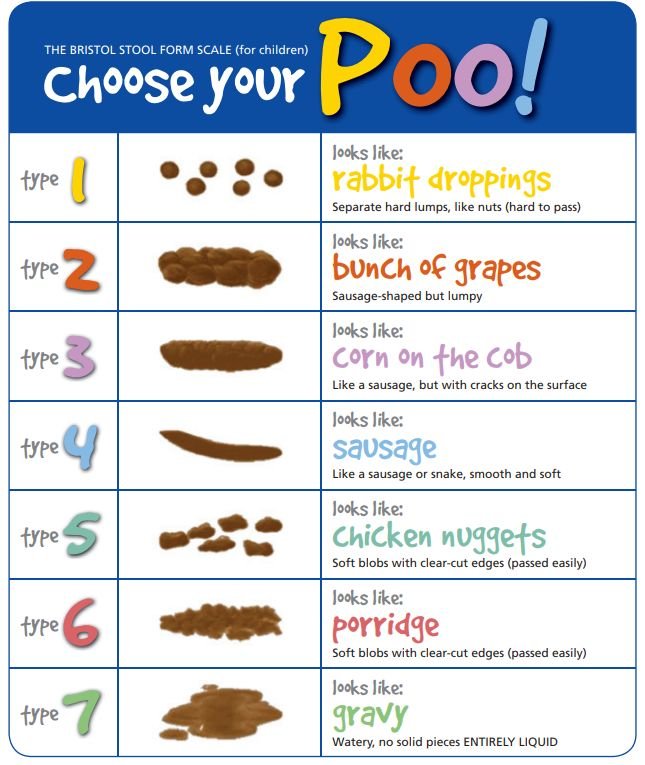
Shaped like a sausage, with cracks on the surface, it looks like a corn on the cob (Bristol Stool Scale Type 3), or
Formed like a snake or sausage, smooth and soft (Bristol Stool Scale Type 4)
Frequency:
Anywhere from three times per day to
Once every three days
Colour:
Brown, varying from light to dark shades
Passed easily, without pain or blood
What is an Abnormal Poop?
Characteristics of abnormal stool and bowel movements:
Shape & Consistency:
Hard and dry, Bristol Stool Chart (Stool type 1 and 2) or
Soft and loose, Bristol Stool Chart (Stool type 5, 6, & 7)
Frequency:
More than three times per day or
Less than once every three days
Colour:
A shade other than brown (e.g., black, red, pale, clay-coloured, green)
Smell abnormally foul or the smell may linger
Red Flag Symptoms
If you experience symptoms that are new, persistent or unexplained, you should see your GP for assessment.
Red flag symptoms include:
Weight loss without trying
Changes in bowel habits
A change in stool shape or consistency
Blood in the stool or rectal bleeding
Incomplete evacuation
Waking at night to pass stool
Frequent gas, pain or cramping
Unexplained anaemia
Abdominal pain or bloating
Fever
Family history of bowel cancer
Bristol Stool Form Scale (for children) or adults with a sense of humour!
WHO EXPERIENCES CONSTIPATION?
According to a 2019 study of Australian adults, 24.0% experience chronic constipation, and 39.6% experience sub-chronic constipation. While everyone with a large bowel can experience constipation, it is more common in women (geez, thanks to female sex hormones!), older individuals, and people with lower incomes.
The positive news is that constipation is a manageable condition, and you can achieve regular and satisfying bowel movements.
HOW IS CONSTIPATION DIAGNOSED?
Occasional constipation can be expected due to changes in routine, travel, or diet. For instance, when travelling and encountering bathroom anxiety due to unfamiliar surroundings, insufficient water intake, and consuming different foods during your journey can contribute to this. Upon reaching your destination, as you settle in and establish a more familiar routine, bowel movements often return to normal. This type of transient constipation typically doesn’t require a visit to your doctor.
It’s good to see your GP for support to resolve your constipation and to rule out any potential more sinister causes of constipation:
It impacts your day-to-day quality of life
It persists for an extended period or occurs suddenly
Or altered bowel movements occur after turning 50
Involves blood in your poo (yes, you should be looking)
It is accompanied by weight loss without trying, even if you think the loss of weight is good.
If there is a family history of bowel disease (cancer, coeliac disease, or inflammatory bowel disease).
CONSTIPATION DIAGNOSTIC CRITERIA
The diagnosis of conditions like irritable bowel syndrome with Constipation (IBS-C), Functional Constipation, and Opioid-Induced Constipation relies on the Rome IV Diagnostic Criteria for Disorder of Gut-Brain Interaction (DGBI).
Irritable Bowel Syndrome (IBS)
Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
Related to defecation
Associated with a change in the frequency of stool
Associated with a change in form (appearance) of stool
Criteria fulfilled for the last 3 months with symptom onset at least 6 months before diagnosis.
IBS with predominant constipation (IBS-C)
More than 25% of Bristol stool types 1 or 2 bowel movements and less than 25% of Bristol stool types 6 or 7.
Functional Constipation
Must include two or more of the following:
Straining during more than 25% of defecations
Lumpy or hard stools more than 25% of defecations
Sensation of incomplete evacuation of more than 25% of defecations
The sensation of anorectal obstruction/blockage more than 25% of defecations
Manual maneuvers to facilitate more than 25% of defecations (e.g., digital evacuation, support of the pelvic floor)
Fewer than three spontaneous bowel movements per week
Loose stools are rarely present without the use of laxatives
Insufficient criteria for irritable bowel syndrome
Criteria fulfilled for the last 3 months with symptoms onset at least 6 months before diagnosis.
Opioid Induced Constipation
New or worsening symptoms of constipation when initiating, changing, or increasing opioid therapy must include two or more of the following:
Straining during more than 25% of defecations
Lumpy or hard stools more than 25% of defecations
Sensation of incomplete evacuation of more than 25% of defecations
The sensation of anorectal obstruction/blockage in more than 25% of defecations
Manual maneuvers to facilitate more than 25% of defecations (e.g., digital evacuation, support of the pelvic floor)
Fewer than three spontaneous bowel movements per week
Loose stools are rarely present without the use of laxatives.
WHAT CAUSES AND CONTRIBUTES TO CONSTIPATION?
Types of Functional Constipation
Normal transit constipation, including irritable bowel syndrome with constipation (most common)
Slow transit constipation (common in women)
Defecatory disorders
Secondary Causes of Constipation:
Organic: colorectal cancer, extra-intestinal mass
Endocrine or metabolic: diabetes mellitus, hypothyroidism, chronic renal insufficiency
Neurological: spinal cord injury, Parkinson’s disease, paraplegia, Hirschsprung’s disease
Anorectal: anal fissure, anal stricture, inflammatory bowel disease
Drugs: opiates, blood pressure medications, some antidepressants, drugs for epilepsy….a long list
Supplements: iron, calcium
Diet: insufficient fluid intake, unbalanced fibre intake, inadequate food intake
Lifestyle: lack of movement, supplements, drug use
Behavioural: withholding, routine, positioning
Psychological: eating disorders, anxiety, depression, stressful life events
EIGHT STRATEGIES FOR MANAGING CHRONIC CONSTIPATION
See your GP to ease your mind, get a referral to see a dietitian, and rule out any serious causes
Stay hydrated by drinking plenty of water and fluids
Consume enough fibre, balancing intake
Move your body; physical activity gets your digestive system moving
Overcome poo fright
Practice relaxation techniques
Consider using a squatty potty (even if you’re not constipated)
If other strategies fail, consult a gut health dietitian for individualised support and dietary advice to help to relieve constipation
How can a Dietitian Help with Constipation
A dietitian can provide valuable support in managing constipation, whether it’s occasional or chronic. This may include:
Exploring possible causes
Personalising fibre recommendations
Strategies for optimising hydration
Guidance around structuring meals and routines
Individualised strategies for symptom management
Ongoing monitoring and support
REFERENCES
Barberio, B., Judge, C., Savarino, E. V., & Ford, A. C. (2021). Global prevalence of functional constipation according to the Rome criteria: a systematic review and meta-analysis. The Lancet Gastroenterology & Hepatology, 6, 8, p638-648.
Judkins, C. P., Wang, Y., Jelinic, M., Bobik, A., Vinh, A., Sobey, C. G., & Drummond, G. R. (2023). Association of constipation with increased risk of hypertension and cardiovascular events in elderly Australian patients. Scientific Reports, 13.
Werth, B. L., Williams, K. A., Fisher, M. J., & Pont, L. G. (2019). Defining constipation to estimate its prevalence in the community: results from a national survey. BMC Gastroenterology, 19, 75.
Werth, B. L., Williams, K. A., Fisher, M. J., & Pont, L. G. (2020). Chronic constipation in the Community: A National Survey of Australian Adults. Journal of Wound, Ostomy and Continence Nursing, 47, 3, p 259-264.