Dieting Understanding the Risks
This post discusses topics (dieting, disordered eating, eating disorders, self-harm and suicidality) that may be distressing for some. Please access support services if required.
The Butterfly National Helpline 1800 33 4673
Eating Disorders Victoria 1300 550 236
Beyond Blue Helpline 1300 22 4636
Call 000 in an emergency
Right now, we’re in a pretty unprecedented time, where diet culture, influencer social marketing media, weight-loss drugs, and weight stigma have all collided.
It’s incredibly disheartening to understand the evidence yet have to witness influencers amplify misinformation and unknowingly cause harm in an already nutrition-confused public. Honestly, the social media ban can’t come soon enough if it means preventing the next generation’s relationship with food and their bodies from being completely derailed.
Dieting is Disordered Eating
The difference between dieting, disordered eating and a diagnosable eating disorder is the frequency and severity of behaviours, the impact on quality of life and medical and psychological complications.
| Dieting Behaviours | Disordered Eating Behaviours |
|---|---|
|
|
Eating Disorders
Dieting is the strongest predictor for the development of an eating disorder.
Prevalence
An estimated 1.1 million Australian’s (4.5%) are currently living with an eating disorder
With 10.5% of the population experiencing an eating disorder at some point in their lifetime
Since 2012, there has been a 21% increase in people impacted by eating disorders
They cost the Federal Government $4.7 billion each year
Women are twice as likely as men to experience an eating disorder
27% were aged under 19 (up from 15% in 2012)
Eating disorders are the third most common chronic illness in young women
Less than one in three people affected will seek help
Eating disorders have the highest mortality rate of any psychiatric illness with 1,273 deaths in Australia in 2023
You do not have to be underweight to die from an eating disorder
Eating disorders don’t discriminate, they can affect anyone, regardless of:
Age (eating disorders have been diagnosed in those younger than 5 years old and older than 80 years old)
Gender
Weight
BMI
Body sizes
Body shape
Skin colour
Culture
Nationality
Financial situation
Education level
Types of Eating Disorders
There’s a common misconception that eating disorders always present as someone being severely underweight, but in reality, this is far from accurate.
Anorexia nervosa (3%)
Bulimia nervosa (12%)
Binge eating disorder (47%)
Others (38%)
| Medical Consequences | Psychological Consequences |
|---|---|
|
|
Weight Cycling (yo-yo dieting)
Weight cycling or yo-yo dieting is repeated weight loss and weight regain, and it drives long-term weight gain, alters body composition toward a greater amount of fat verse lean muscle mass and increases inflammation.
Chronic weight loss and weight regain increases the risk for:
Hypertension (high blood pressure)
Hyperlipidaemia
Cardiovascular disease (heart disease)
All-cause mortality (death from any cause)
Obstructive sleep apnoea
Metabolic dysfunction-associated steatotic liver disease
Type 2 diabetes
Heart failure
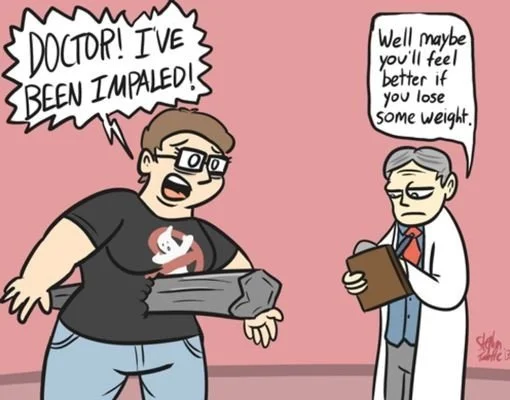
Weight Stigma
Weight stigma is the discrimination toward people based on their body weight and size.
Weight stigma is particularly pervasive in healthcare. As a result of weight stigma and discrimination, people with higher weight as more likely to:
avoid seeking and engaging in medical care, leading to delays in diagnosis and treatment
engage in disordered eating, contributing the onset of eating disorder and increasing disordered eating in people experiencing eating disorders
experience higher levels of body dissatisfaction
experience higher levels of psychological distress, including stress, anxiety, depression, feelings of worthlessness and loneliness, and suicidal ideation
experience poorer quality of life
face discrimination in healthcare, affecting the quality of care they receive, leading to poorer health outcomes and increasing risk of mortality
face discrimination in employment and education
avoid physical activity and leisure pursuits
Weight stigma and discrimination have been shown to be associated with weight gain over the longer term, independent of the person’s baseline weight.
Weight stigma experienced from a health professional increase the following after controlling for BMI, health care delay or avoidance, sedentary behaviour, and selected demographic characteristics:
High blood pressure (Hypertension)
High blood sugar (Hyperglycaemia)
Any arthritis
Non-arthritic chronic pain
Infertility
Healthcare concern discounted
Eating disorders
A Non-Diet Approach is:
A whole person approach
Health-focused
Harm reduction
Protective against the development of an eating disorder
An inclusive approach
Behaviour focused and weight isn’t a behaviour it’s an outcome
References
Impact of weight bias and stigma on quality of care and outcomes for patients with obesity - PMC