Low FODMAP Diet
What Does FODMAP Mean?
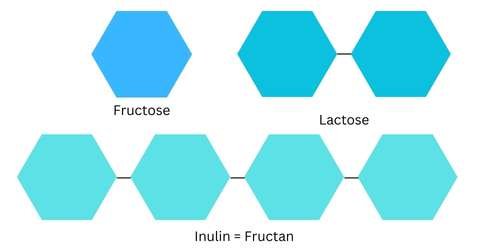
FODMAP is an acronym for groups of short-chain carbohydrates (sugars).
Fermentable
Oligosaccharides —> Oligo = few, saccharide = sugar
Disaccharides —> Di = 2, saccharide = sugar
Monosaccharides —>Mono = 1, saccharide = sugar
and
Polyols —> Poly = many, ols = sugar alcohol (not the boozy type)
The numbers 1, 2, and few are referring to the amount of sugar molecules joined together.
Then we break it down some more.
O —> Fructans (FOS), Galactans (GOS)
D —> Lactose
M —> Fructose (excess)
P —> Sorbitol, Mannitol (naturally in foods), Xylitol, Maltitol (additives)
These sugars are naturally present in a wide variety of foods that are beneficial for our overall health. FODMAPs are not efficiently absorbed in the small intestine, allowing them to make their way to the large intestine. There are two processes that occur when eating high-FODMAP foods:
1. They draw water into the intestine, expanding the bowel and increasing pressure.
2. They undergo fermentation by gut bacteria, resulting in an increase in gas production.
Both of these responses are normal physiological responses to FODMAP-rich foods. However, in individuals with a sensitive gut (such as those with IBS), these processes can lead to stomach distension, bloating, excessive gas, and altered bowel habits (constipation/diarrhoea). Not a pleasant experience!
How Can A Dietitian Help With IBS?
A dietitian that is trained and specialising in IBS will:
Look at the whole picture
Ensure that you have received a confirmed IBS diagnosis from a doctor
Identify any concerning symptoms and refer you to your GP for medical assessment
Be comfortable discussing bowel movements and will enquire about all relevant details, appreciating a good sense of humour when discussing challenging subjects.
Acknowledge that FODMAPs aren’t the sole dietary triggers for gastrointestinal symptoms
Recognise various non-food factors influencing gastrointestinal symptoms, including stress, mental health, the gut-brain axis, medication side effects, hormonal fluctuations, menstruation, and pelvic floor issues.
Always prioritise the least restrictive dietary pattern.
Guarantee that you’re following a balanced diet that meets your needs.
WHAT IS THE LOW FODMAP DIET?
The FODMAP diet was originally developed in Australia by the team at Monash University in Melbourne, Victoria. It comprises a three-phase process aimed at determining an individual’s sensitivity to FODMAP foods. The primary goal is to strike a balance between symptom management and minimising dietary restrictions.
1. Phase 1 – FODMAP restriction (2-6 weeks)
The primary objective of this phase is to ascertain whether an individual is sensitive to FODMAPs. During this period, high-FODMAP foods are replaced with low-FODMAP alternatives, with the anticipation of observing a reduction in symptoms within two weeks.
2. Phase 2 – FODMAP reintroduction (6-8 weeks)
In this phase, the focus is on identifying which specific FODMAP groups an individual may be sensitive to. FODMAP subgroups are methodically reintroduced, and any resultant symptom responses are meticulously recorded.
3. Phase 3 – FODMAP personalisation (long-term)
The ultimate aim of this phase is to expand an individual's diet and establish a personalised, sustainable dietary pattern. Well-tolerated FODMAP groups are included, while only poorly tolerated FODMAP foods are restricted. It is important to note that regularly challenging poorly tolerated FODMAP groups over time is crucial, as tolerance levels and symptoms may change.
WHAT IS THE EVIDENCE FOR A LOW FODMAP DIET?
Scientific research has demonstrated that the low FODMAP diet can provide symptom relief to 75% of individuals suffering from irritable bowel syndrome (IBS).
HOW LONG SHOULD I FOLLOW A LOW FODMAP DIET?
If you are independently following a Low FODMAP diet and have not experienced symptom relief within two weeks, it is advisable to seek guidance from a FODMAP-trained dietitian.
Phase 1 of the diet should not extend beyond six weeks.
Phase 2 should be limited to a duration of 6-8 weeks.
As for Phase 3, this involves a personalized dietary approach intended for long-term adoption. Nevertheless, it is strongly recommended to periodically reintroduce poorly tolerated FODMAP subgroups over time.
ARE THERE ANY ISSUES WITH FOLLOWING A LOW FODMAP DIET?
When evaluating an individual’s dietary patterns, it’s important to consider the broader context. Any dietary intervention can be executed well or poorly, underscoring the importance of ensuring that all essential nutrients are being consumed. Unnecessary restrictions on foods, particularly those crucial for maintaining not only good physical health but also mental health, should be avoided. It’s worth noting that foods containing FODMAPs also provide other essential macro and micronutrients, including prebiotic fibres that are highly favoured by gut bacteria. Through the process of fermenting these prebiotic fibres, our gut bacteria generate metabolites that confer beneficial health effects to us, the host.
Making informed food choices can be quite challenging, even in typical circumstances. Incorporating a restrictive diet into the mix can make tasks like grocery shopping, meal planning, and dining out even more complex. Therefore, it’s imperative to approach this process with caution and choose the least restrictive path possible.
Furthermore, it’s essential to comprehend how specific FODMAP-rich foods may trigger gastrointestinal symptoms in certain individuals, all while avoiding stigmatising particular food components and entire food groups such as gluten or dairy. In such situations, seeking guidance from a knowledgeable professional who empathises with this challenge can be highly beneficial.
Taking into account the psychological impact of both experiencing symptoms associated with irritable bowel syndrome (IBS) and adhering to a restrictive dietary intervention is crucial. Achieving a delicate balance is essential to mitigate potential harm, including the risk of developing an eating disorder or disordered eating.
WHAT FOODS ARE HIGH IN FODMAPS?
FOS (fructo-oligosaccharides) —> Dates, dried figs, onion, garlic, artichoke, pasta, rye, wheat
GOS (galacto-oligosaccharides)—> Green peas, baked beans, black beans, cashews
Sorbitol —> Apple, pear, avocado, lychee, sugar free lollies
Mannitol —> Mushrooms, cauliflower, celery
Excess Fructose —> Apple, mango, grapes, watermelon, asparagus, honey, fruit juice
Lactose —> Cow’s milk, yoghurt, custard, ice-cream
WHAT FOODS ARE LOW FODMAP?
Vegetables: Beans, Brussels sprouts, carrots, corn, potatoes,
Fruits: Blueberries, kiwi fruit, strawberries
Protein: All plain meats, seafood, firm tofu, tempeh
Grains: Spelt sourdough, rice noddles, oats, polenta, corn tortilla
Dairy products: Hard cheeses, cream
Fats: All fats and oils
Nuts: Almonds, peanuts, walnuts
Drinks: Tea, coffee
LEARN MORE ABOUT GUT HEALTH
IBS Symptoms, Diet & Management | Dietitian Guide — Melbourne Dietitian & Nutritionist
How Are Farts Made? Understanding Gas & Digestion — Melbourne Dietitian & Nutritionist
What Is a Normal Stool? A Dietitian Explains — Melbourne Dietitian & Nutritionist